Hernia- Open Inguinal Hernia Repair
- Home
- Hernia- Open Inguinal Hernia Repair
What do I need to know about this condition?
A hernia, sometimes referred to as a rupture, occurs when a part of an internal organ, sometimes the bowel, pushes through a weak point in the abdominal wall.
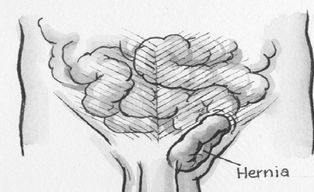
An Inguinal Hernia
Inguinal hernia is the most common type of hernia, and twenty times more common in men than in women. It is likely that about 1 in 20 men will develop an inguinal hernia. The inguinal canal is in the groin. The first signs of a hernia are pain and/or a lump.
What do I need to know about this Procedure?
Open surgery is performed under a general, spinal or local anaesthetic to repair the weakness in the abdominal wall.
A small cut is made at the site of the hernia. The weak area is repaired. Sometimes the weak area is reinforced with mesh.
What are the benefits of having this procedure?
The pain and lump will be relieved by the surgery. Planned surgical treatment of a hernia is much safer than leaving the hernia until an emergency happens.
What are the risks of not having this procedure?
The hernia will probably get bigger. Inside, the bowel may become trapped and blocked or gangrenous (that part of the bowel dies). This can be very dangerous and will need emergency treatment. Treatment may require extensive surgery to the bowel.
What are some alternative treatments?
A truss may be worn which applies support to the weak area. The truss is not a cure and can be uncomfortable. It may cause pressure sores and is not always effective. The proper use of a truss enquires medical advice.
My Aneasthetic
This procedure will require an anaesthetic.
What are the risks of this specific procedure?
There are risks and complications with this procedure.
They include but are not limited to the following.
General risks:
- Infection can occur, requiring antibiotics and further treatment.
- Bleeding could occur and may require a return to the operating room. Bleeding is more common if you have been taking blood thinning drugs such as Warfarin, Asprin, Clopidogrel (Plavix or Iscover) or Dipyridamole (Persantin or Asasantin).
- Small areas of the lung can collapse, increasing the risk of chest infection. This may need antibiotics and physiotherapy.
- Increased risk in obese people of wound infection, chest infection, heart and lung complications, and thrombosis.
- Heart attack or stroke could occur due to the strain on the heart.
- Blood clot in the leg (DVT) causing pain and swelling. In rare cases part of the clot may break off and go to the lungs.
- Death as a result of this procedure is possible.
Specific risks
- Trouble passing urine after the operation
A temporary problem due to spasm of the bladder muscles in 1 in 100. More common in elderly males. A catheter (plastic tube) is put into the bladder to drain the urine away. - Swelling of the testicle and scrotum
In male patients, the testicle and the contents of the scrotum may swell due to tissue damage during surgery or bleeding during or after surgery. Also the penis may show bruising. The swelling of the scrotum may be drained using a needle. The testicle may stop making sperm and it may shrink (1 in 3000 to 1 in 200 for primary repairs and 1 in 20 to 1 in 120 for recurrent repairs). - Injury to sperm tube (Vas Deferens)
The tube carrying sperm from the testicle to the prostate may be injured which may reduce fertility in 1 in 100. Results in partial vasectomy. - Ongoing pain or discomfort in groin
One of the small nerves in the groin can be cut or caught in a stitch or scar causing long term burning and aching in the groin in 1 in 50. This may happen straight after surgery or months or years later. - Change to testicle
The testicle may sit a little higher in the scrotum after surgery. A change in physical appearance. - Wound infection
The wound may become infected. The rate of risk is estimated at about 1% or 1 in 100. Wound infections are usually treated with dressings and/or antibiotics. - Bleeding into the wound
Possible bleeding into the wound after the surgery in 1 in 30. Swelling, bruising, blood stained discharge, which may cause pain, or become infected. Treatment is usually antibiotics and/or drainage by further surgery. - The wounds may not heal normally
The scars can thicken and turn red and may be painful. This is permanent and can be disfiguring. It is more frequent in recurrent hernias. - Bands of scar tissue –adhesions
Bands of scar tissue can form inside the abdomen, which may cause bowel blockage and possible bowel damage. Further surgery may be necessary. - Hernia comes back
The hernia may come back in 1 in 30 to 1 in 100. Further surgery may be needed to repair the hernia. - Hernias at the wound sites
Hernias may form where instruments were passed into the abdomen. This may need further surgery. - Increased risk in smokers
Smoking slows wound healing and affects the heart, lungs and circulation. Giving up smoking before the operation will help reduce the risk. - Death is extremely rare due to hernia repair – less than 1 in 10,000.