Percutaneous Endoscopic Gastrostomy (PEG) Tube
- Home
- Percutaneous Endoscopic Gastrostomy (PEG) Tube
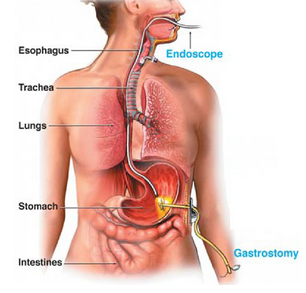
What is a percutaneous endoscopic gastrostomy (PEG) tube?
PEG stands for Percutaneous (through the skin) Endoscopic (using an endoscopic instrument which is a long thin tube with a small camera and light attached which allows the doctor to see the pictures of the inside of your gut on the video screen ) and Gastrostomy (means to the stomach). The doctor creates a hole in the tummy (abdominal wall) to allow a feeding tube to be inserted directly into the stomach.
 The feeding tube is placed in people who require long term nutritional support because they are unable to eat food normally.
The feeding tube is placed in people who require long term nutritional support because they are unable to eat food normally.
This procedure can also be performed to shrink the stomach in cases of a bowel obstruction.
The doctor will give you an injection of local anaesthetic into the skin. A needle is then passed through the skin (just under the ribs on the left side of the abdomen) down into the stomach. A wire is inserted into the needle and used to guide the tube through the mouth into position in the stomach.
This procedure may or may not require a sedation anaesthetic.
Will there be any discomfort? Is any anaesthetic needed?
The procedure can be uncomfortable and to make the procedure more comfortable a sedative injection or a light anaesthetic will be given.
Before the procedure begins, the doctor will put a drip into a vein in your hand or forearm. This is where the sedation or anaesthetic is injected.
What is sedation?
Sedation is the use of drugs that give you a ‘sleepy like’ feeling. It makes you feel very relaxed during a procedure that may be otherwise unpleasant or painful.
You may remember some or little about what has occurred during the procedure.
Anaesthesia is generally very safe but every anaesthetic has a risk of side effects and complications. Whilst these are usually temporary, some of them may cause long-term problems.
The risk to you will depend on:
personal factors, such as whether you smoke or are overweight.
whether you have any other illness such as asthma, diabetes, heart disease, kidney disease, high blood pressure or other serious medical conditions.
What are the risks of this specific procedure?
There are risks and complications with this procedure.
They include but are not limited to the following.
Common risks and complications include:
- Nausea and vomiting.
- Faintness or dizziness, especially when you start to move around.
- Headache
- Pain, redness or bruising at the sedation injection (usually in the hand or arm).
- Muscle aches and pains.
- Allergy to medications given at time of the procedure.
- Failure of local anaesthetic. This may require a further injection of anaesthetic or a different method of anaesthetic to be used.
Uncommon risks and complications include:
- Infection at the stoma site. This will need antibiotics.
- Bleeding from the wound or with the abdomen.
- Damage to other organs within the abdomen during insertion of the PEG tube.
- Peritonitis from leakage of fluid from the stomach or from an infection
- Heart and lung problems such as heart attack or vomit in the lungs causing pneumonia.
- Emergency treatment may be necessary.
- Damage to your teeth or jaw due to the presence of instruments in your mouth.
- ‘Dead arm’ type feeling in any nerve, due to positioning with the procedure – usually temporary.
- An existing medical condition that you may have getting worse.
- The procedure may not be successful.
Rare risks and complications include:
- Bacteraemia (infection of the blood). This will need antibiotics.
- Anaphylaxis (severe allergy) to medication given at the time of procedure.
- Death as a result of complications to this procedure is rare.
What are you responsibilities before having this procedure?
You are less at risk of problems if you do the following:
- Bring all your prescribed drugs, those drugs you buy over the counter, herbal remedies and supplements and show your doctor what you are taking. Tell your doctor about any allergies or side effects that you may have.
- Do not drink any alcohol and stop recreational drugs 24 hours before the procedure. If you have a drug habit please tell your doctor.
- If you take Warfarin, Persantin, Clopidogrel (Plavix or Iscover), Asasantin or any other drug that is used to thin your blood ask your doctor if you should stop taking it before the procedure as it may affect your blood clotting. Do not stop taking them without asking your doctor.
Tell your doctor if you have:
- had heart valve replacement surgery.
- received previous advice about taking antibiotics before a dental treatment or a surgical
- procedure. If so you may also need antibiotics before the PEG tube.
Preparation for the procedure
There are some limits with eating and drinking before having the procedure. Your doctor will discuss this with you. You may also be given antibiotics on the day of the procedure to reduce the risk of infection at the stoma site.
Feeding through the PEG tube
Clear fluids, often water, will be given initially through the PEG tube 6-24 hours after its insertion. Once this is tolerated, then feeds and medications may be given through the tube. Medications can also be given through the PEG tube but care is needed as some medications can clog up the tubing. Your pharmacist will advise you with this.
What care does the PEG tube need?
Clear fluids, often water, will be given initially through the PEG tube 6-24 hours after its insertion. Once this is tolerated, then feeds and medications may be given through the tube. Medications can also be given through the PEG tube but care is needed as some medications can clog up the tubing. Your pharmacist will advise you with this.
How long does the PEG tube last?
This depends on the type of tube you have inserted, and how it is looked after.
A PEG tube can last up to a year but will need to be changed every so often due to the stomach acids.
The tubes can become blocked by food, residue or medications. It should be flushed well after each use.
If the PEG tube falls out, it is important to have another tube placed as soon as possible to prevent the hole closing over.
The PEG tube can be replaced by another tube or by a low profile device, also called a ‘Mic-Key’. You should discuss this option with your doctor when your PEG tube is due to be changed.
If the PEG tube is no longer needed it can be simply removed and the exit hole will quickly close over. Sometimes it may require a small operation by a surgeon to repair the hole once the tube is removed.
What are the risks of a PEG tube?
When the PEG tube is used for feeding there are 2major common risks;
the feeding tube may become dislodged or blocked by medications or feeding fluid and you can get pneumonia if you aspirate any of the feeding fluid.
What are the safety issues?
Sedation will affect your judgment for about 24 hours.
For your own safety and in some cases legally;
- Do NOT drive any type of car, bike or other vehicle. You must be taken home by a responsible adult person.
- Do NOT operate machinery including cooking implements.
- Do NOT make important decisions or sign a legal document.
- Do NOT drink alcohol, take other mind-altering substances, or smoke. They may react with the sedation drugs.
- Have an adult with you on the first night after your surgery.
Notify the hospital Emergency Department straightaway if you have;
- severe ongoing abdominal pain
- a fever
- sharp chest or throat pain
- redness, tenderness or swelling for more than 48hours where you had the injection for
- sedation (either in the hand or arm).
If your PEG tube falls out contact the hospital straight away so that it can be replaced before your wound closes.